An undescended testicle (cryptorchidism) is a testicle that hasn’t moved into its proper position in the bag of skin hanging below the penis (scrotum) before birth. Usually just one testicle is affected, but about 10 percent of the time both testicles are undescended.
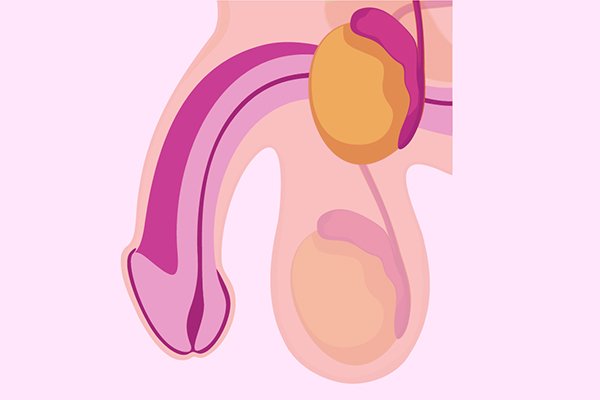
Testicles form in the abdomen during fetal development. During the last couple of months of normal fetal development, the testicles gradually descend from the abdomen through a tube-like passageway in the groin (inguinal canal) into the scrotum. With an undescended testicle, that process stops or is delayed.
An undescended testicle is uncommon in general, but common among baby boys born prematurely.
Older boys — from infants to pre-adolescent boys — who have normally descended testicles at birth might appear to be “missing” a testicle later. This condition might indicate:
- A retractile testicle, which moves back and forth between the scrotum and the groin and might be easily guided by hand into the scrotum during a physical exam. This is not abnormal and is due to a muscle reflex in the scrotum.
- An ascending testicle, or acquired undescended testicle, that has “returned” to the groin and can’t be easily guided by hand into the scrotum.
Symptoms
Not seeing or feeling a testicle where you would expect it to be in the scrotum is the main sign of an undescended testicle.
Causes
The exact cause of an undescended testicle isn’t known. A combination of genetics, maternal health and other environmental factors might disrupt the hormones, physical changes and nerve activity that influence the development of the testicles.
Risk factors
Factors that might increase the risk of an undescended testicle in a newborn include:
- Low birth weight
- Premature birth
- Family history of undescended testicles or other problems of genital development
- Conditions of the fetus that can restrict growth, such as Down syndrome or an abdominal wall defect
- Alcohol use by the mother during pregnancy
- Cigarette smoking by the mother or exposure to secondhand smoke
- Parents’ exposure to some pesticides
Complications
In order for testicles to develop and function normally, they need to be slightly cooler than normal body temperature. The scrotum provides this cooler environment. Complications of a testicle not being located where it is supposed to be include:
- Testicular cancer.Testicular cancer usually begins in the cells in the testicle that produce immature sperm. What causes these cells to develop into cancer is unknown. Men who’ve had an undescended testicle have an increased risk of testicular cancer.
The risk is greater for undescended testicles located in the abdomen than in the groin, and when both testicles are affected. Surgically correcting an undescended testicle might decrease, but not eliminate, the risk of future testicular cancer.
- Fertility problems.Low sperm counts, poor sperm quality and decreased fertility are more likely to occur among men who’ve had an undescended testicle. This can be due to abnormal development of the testicle, and might get worse if the condition goes untreated for an extended period of time.
Other complications related to the abnormal location of the undescended testicle include:
- Testicular torsion.Testicular torsion is the twisting of the spermatic cord, which contains blood vessels, nerves and the tube that carries semen from the testicle to the penis. This painful condition cuts off blood to the testicle.
If not treated promptly, this might result in the loss of the testicle. Testicular torsion occurs 10 times more often in undescended testicles than in normal testicles.
- If a testicle is located in the groin, it might be damaged from pressure against the pubic bone.
- Inguinal hernia.If the opening between the abdomen and the inguinal canal is too loose, a portion of the intestines can push into the groin.
Diagnosis
The doctor might recommend surgery for diagnosis and potential treatment of an undescended testicle as follows:
- A small tube containing a camera is inserted through a small incision in the abdomen. Laparoscopy is done to locate an intra-abdominal testicle.
The doctor might be able to fix the undescended testicle during the same procedure, but an additional surgery might be needed in some cases. Alternatively, laparoscopy might show no testicle present, or a small remnant of nonfunctioning testicular tissue that is then removed.
- Open surgery.Direct exploration of the abdomen or groin through a larger incision might be necessary in some cases.
After birth, if the doctor can’t detect any testicles in the scrotum, he or she might order further testing to determine if the testicles aren’t there at all rather than undescended. Some conditions that result in absent testicles can cause serious medical problems soon after birth if left undiagnosed and untreated.
Imaging tests, such as an ultrasound and MRI, generally aren’t recommended for diagnosing an undescended testicle.
Treatment
The goal of treatment is to move the undescended testicle to its proper location in the scrotum. Treatment before 1 year of age might lower the risk of complications of an undescended testicle, such as infertility and testicular cancer. Earlier is better, but it’s recommended that surgery takes place before the child is 18 months old.The vast majority of the time, the undescended testicle moves into the proper position on its own, within the first few months of life. If the undescended testicle that doesn’t correct itself, surgery can relocate the testicle into the scrotum.
- Surgery
An undescended testicle is usually corrected with surgery. The surgeon carefully manipulates the testicle into the scrotum and stitches it into place (orchiopexy). This procedure can be done either with a laparoscope or with open surgery.Orchiopexy, the most common surgical procedure for correcting a single descending testicle, has a success rate of nearly 100 percent. Fertility for males after surgery with a single undescended testicle is nearly normal, but falls to 65 percent in men with two undescended testicles. Surgery might reduce the risk of testicular cancer, but does not eliminate it.
The type of surgery will depend on a number of factors, such as the health of the patient and how difficult the procedure might be. The surgeon will likely recommend doing the surgery when the baby is about 6 months old and before he is 12 months old. Early surgical treatment appears to lower the risk of later complications.
In some cases, the testicle might be poorly developed, abnormal or dead tissue. The surgeon will remove this testicular tissue.
If the patient also has an inguinal hernia associated with the undescended testicle, the hernia is repaired during the surgery.
After surgery, the surgeon will monitor the testicle to see that it continues to develop, function properly and stay in place. Monitoring might include:
- Physical exams
- Ultrasound exams of the scrotum
- Tests of hormone levels
- Hormone treatment
Hormone treatment is not usually recommended because it is much less effective than surgery.If the patient doesn’t have at least one healthy testicle, the doctor will refer him to a hormone specialist (endocrinologist) to discuss future hormone treatments that would be necessary to bring about puberty and physical maturity.
- Other treatments
If the patient doesn’t have one or both testicles — because one or both are missing or didn’t survive after surgery —saline testicular prostheses for the scrotum that can be implanted during late childhood or adolescence might be an option. These prostheses give the scrotum a normal appearance.