What are the causes of kidney stones?
Kidney stones often have no definite, single cause, although several factors may increase your risk. Kidney stones form when your urine contains more crystal-forming substances — such as calcium, oxalate and uric acid — than the fluid in your urine can dilute. At the same time, your urine may lack substances that prevent crystals from sticking together, creating an ideal environment for kidney stones to form.
Types of kidney stones
- Calcium stones.Most kidney stones are calcium stones, usually in the form of calcium oxalate. Oxalate is a naturally occurring substance found in food and is also made daily by your liver. Some fruits and vegetables, as well as nuts and chocolate, have high oxalate content.
Dietary factors, high doses of vitamin D, intestinal bypass surgery and several metabolic disorders can increase the concentration of calcium or oxalate in urine.
Calcium stones may also occur in the form of calcium phosphate. This type of stone is more common in metabolic conditions, such as renal tubular acidosis. It may also be associated with certain migraine headaches or with taking certain seizure medications, such as topiramate.
- Struvite stones.Struvite stones form in response to an infection, such as a urinary tract infection. These stones can grow quickly and become quite large, sometimes with few symptoms or little warning.
- Uric acid stones.Uric acid stones can form in people who don’t drink enough fluids or who lose too much fluid, those who eat a high-protein diet, and those who have gout. Certain genetic factors also may increase your risk of uric acid stones.
- Cystine stones.These stones form in people with a hereditary disorder that causes the kidneys to excrete too much of certain amino acids (cystinuria).
Are there any risk factors for the development of kidney stones?
Factors that increase your risk of developing kidney stones include:
- Family or personal history.If someone in your family has kidney stones, you’re more likely to develop stones, too. And if you’ve already had one or more kidney stones, you’re at increased risk of developing another.
- Not drinking enough water each day can increase your risk of kidney stones. People who live in warm climates and those who sweat a lot may be at higher risk than others.
- Certain diets.Eating a diet that’s high in protein, sodium (salt) and sugar may increase your risk of some types of kidney stones. This is especially true with a high-sodium diet. Too much salt in your diet increases the amount of calcium your kidneys must filter and significantly increases your risk of kidney stones.
- Being obese.High body mass index (BMI), large waist size and weight gain have been linked to an increased risk of kidney stones.
- Digestive diseases and surgery.Gastric bypass surgery, inflammatory bowel disease or chronic diarrhea can cause changes in the digestive process that affect your absorption of calcium and water, increasing the levels of stone-forming substances in your urine.
- Other medical conditions.
- a blockage of the urinary tract
- cystic kidney diseases, which are disorders that cause fluid-filled sacs to form on the kidneys
- cystinuria
- gout, a disorder that causes painful swelling of the joints
- hypercalciuria, a condition that runs in families in which urine contains unusually large amounts of calcium; this is the most common condition found in people who form calcium stones
- hyperoxaluria, a condition in which urine contains unusually large amounts of oxalate
- hyperparathyroidism, a condition in which the parathyroid glandsrelease too much parathyroid hormone, causing extra calcium in the blood
- hyperuricosuria, a disorder in which too much uric acid is in the urine
- obesity
- repeated, or recurrent, UTIs
- renal tubular acidosis, a disease that occurs when the kidneys fail to remove acids into the urine, which causes a person’s blood to remain too acidic
· Medicines: You are more likely to develop kidney stones if you are taking one or more of the following medicines over a long period of time:
- diuretics, often called water pills, which help rid your body of water, used in patients with heart failure and hypertension
- calcium-based antacids
- topiramate, used for the treatment of seizures/epilepsy
What are the symptoms of kidney stones?
A kidney stone may not cause symptoms until it moves around within your kidney or passes into your ureter — the tube connecting the kidney and bladder. At that point, you may experience these signs and symptoms:
- Severe pain in the side and back, below the ribs
- Pain that radiates to the lower abdomen and groin
- Pain that comes in waves and fluctuates in intensity
- Pain on urination
- Pink, red or brown urine
- Cloudy or foul-smelling urine
- Nausea and vomiting
- Persistent need to urinate
- Urinating more often than usual
- Fever and chills if an infection is present
- Urinating small amounts
Pain caused by a kidney stone may change — for instance, shifting to a different location or increasing in intensity — as the stone moves through your urinary tract.
When should I consider visiting a doctor?
Seek immediate medical attention if you experience:
- Pain so severe that you can’t sit still or find a comfortable position
- Pain accompanied by nausea and vomiting
- Pain accompanied by fever and chills
- Blood in your urine
- Difficulty passing urine
How can kidney stones be diagnosed?
If your doctor suspects you have a kidney stone, s/he may advise diagnostic tests and procedures, such as:
- Blood testing.Blood tests may reveal too much calcium or uric acid in your blood. Blood test results help monitor the health of your kidneys and may lead your doctor to check for other medical conditions.
- Urine testing.The 24-hour urine collection test may show that you’re excreting too many stone-forming minerals or too few stone-preventing substances. For this test, your doctor may request that you perform two urine collections over two consecutive days.
- Imaging tests may show kidney stones in your urinary tract. Options range from simple abdominal X-rays, which can miss small kidney stones, to high-speed or dual energy computerized tomography (CT) that may reveal even tiny stones.
Other imaging options include an ultrasound, a noninvasive test, and intravenous urography, which involves injecting dye into an arm vein and taking X-rays (intravenous pyelogram) or obtaining CT images (CT urogram) as the dye travels through your kidneys and bladder.
- Analysis of passed stones.You may be asked to urinate through a strainer to catch stones that you pass. Lab analysis will reveal the makeup of your kidney stones. Your doctor uses this information to determine what’s causing your kidney stones and to form a plan to prevent more kidney stones.
What is the treatment for kidney stones?
The treatment for kidney stones varies, depending on the type of stone and the cause.
Small stones with minimal symptoms
Most small kidney stones won’t require invasive treatment. You may be able to pass a small stone by:
- Drinking water.Drinking as much as about 2-3 liters a day may help flush out your urinary system. Unless your doctor tells you otherwise, drink enough fluid — mostly water — to produce clear or nearly clear urine.
- Pain relievers.Passing a small stone can cause some discomfort. To relieve mild pain, your doctor may recommend pain relievers.
- Medical therapy.Your doctor may give you a medication to help pass your kidney stone which relaxes the muscles in your ureter, helping you pass the kidney stone more quickly and with less pain.
Large stones and those that cause symptoms
Kidney stones that can’t be treated with conservative measures — either because they’re too large to pass on their own or because they cause bleeding, kidney damage or ongoing urinary tract infections — may require more-extensive treatment. Procedures may include:
1. Using sound waves to break up stones(Extracorporeal Shock Wave Lithotripsy (ESWL))
The introduction of extracorporeal shock wave lithotripsy (ESWL) in the early 1980s revolutionized the treatment of patients with kidney stone disease. Patients who once required major surgery to remove their stones could be treated with ESWL, and not even require an incision. As such, ESWL is the only non-invasive treatment for kidney stones, meaning no incision or internal telescopic device is required.

ESWL involves the administration of a series of shock waves generated by a machine called a lithotripter. The shock waves are focused by x-ray onto the kidney stone and travel into the body through skin and tissue, reaching the stone where they break it into small fragments. For several weeks following treatment, those small fragments are passed out of the body in the urine.
The procedure lasts about 45 to 60 minutes and can cause moderate pain, so you may be under sedation or light anesthesia to make you comfortable.ESWL can cause blood in the urine, bruising on the back or abdomen, bleeding around the kidney and other adjacent organs, and discomfort as the stone fragments pass through the urinary tract.
Advantages of ESWL
The primary advantage of ESWL is that it is completely non-invasive.
Who should be treated with ESWL?
ESWL is well suited to patients with small kidney stones that can be easily seen by x-ray.
ESWL is NOT a particularly good treatment for:
- Pregnant patients
- Patients on blood thinners or patients with bleeding disorders. Aspirin or other blood thinners must be discontinued for at least 1 week before ESWL.
- Patients with chronic kidney infection, as some fragments may not pass, so the bacteria will not be completely eliminated from the kidney.
- Patients with obstruction or scar tissue in the ureter, which may prevent stone fragments from passing.
- Patients who require immediate and/or complete clearance of stone material.
- Patients with stones composed of cystine and certain types of calcium, as these stones do not fragment well with ESWL
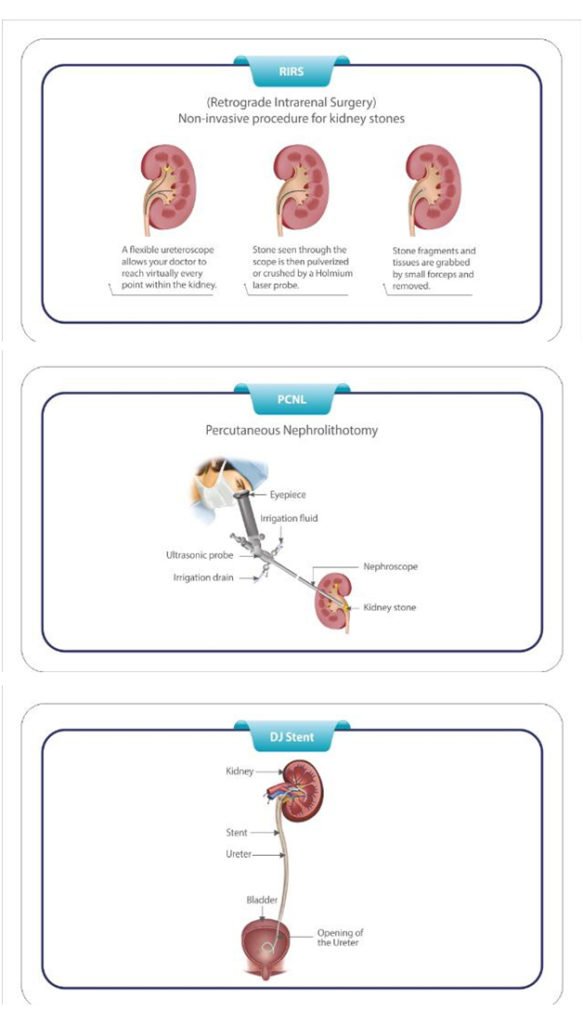
- Cystoscopy and ureteroscopy.During cystoscopy, the doctor uses a cystoscope to look inside the urethra and bladder to find a stone in your urethra or bladder. During ureteroscopy, the doctor uses a ureteroscope, which is longer and thinner than a cystoscope, to see detailed images of the lining of the ureters and kidneys. The doctor inserts the cystoscope or ureteroscope through the urethra to see the rest of the urinary tract. Once the stone is found, the doctor can remove it or break it into smaller pieces. The doctor performs these procedures in the hospital with anesthesia. You can typically go home the same day.After these procedures, sometimes the urologist may leave a thin flexible tube, called a ureteral stent, in your urinary tract to help urine flow or a stone to pass. Once the kidney stone is removed, your doctor sends the kidney stone or its pieces to a lab to find out what type it is.

- Percutaneous nephrolithotomy (PCNL) (surgery to remove very large stones in the kidney)A procedure called percutaneous nephrolithotomy involves surgically removing a kidney stone using small telescopes and instruments inserted through a small incision in your back.You will receive general anesthesia during the surgery and be in the hospital for one to two days while you recover. Your doctor may recommend this surgery if ESWL was unsuccessful.PCNL is a technique used to remove certain stones in the kidney or upper ureter (the tube that drains urine from the kidney to the bladder) that are too large for other forms of stone treatment such as shock wave lithotripsy or ureteroscopy.

Typically, the length of the surgery is three to four hours. The surgery is performed by making a small 1 cm incision in the patient’s flank area. A tube is placed through the incision into the kidney under x-ray guidance. A small telescope is then passed through the tube in order to visualize the stone, break it up and remove it from the body. If necessary a laser or other device called a lithotripter may be used to break up the stone before it can be removed. This procedure has resulted in significantly less post-operative pain, a shorter hospital stay, and earlier return to work and daily activities when compared to open stone surgery.
This technique also has a higher success rate for clearing all stones in one setting than other techniques such as extracorporeal shock wave lithotripsy (ESWL), which often require several attempts.
Potential Risks and Complications
Although this procedure has proven to be very safe, as in any surgical procedure there are risks and potential complications. The safety and complication rates are similar when compared to the open surgery. Potential risks include:
- Bleeding: Some blood loss will occur with this procedure but rarely do patients require a blood transfusion. If you are interested in autologous blood transfusion (donating your own blood) you must make your surgeon aware. When the packet of information is mailed to you regarding your surgery, you will also receive an authorization form for you to take to the Red Cross. You must coordinate this with the Red Cross in your area.
- Infection: All patients are treated with broad-spectrum antibiotics to decrease the chance of infection from occurring after surgery. If you develop any signs or symptoms of infection after the surgery (fever, drainage from incision, urinary frequency or discomfort, pain or anything that you may be concerned about) please contact us at once.
- Tissue / Organ Injury: Although uncommon, possible injury to surrounding tissue/organs including bowel, vascular structures, spleen, liver, lung, pancreas and gallbladder could require further surgery. Loss of kidney function is rare but is a potential risk. Scar tissue may also form in the kidney or ureter requiring further surgery.
- Conversion to open surgery: This surgical procedure may require conversion to the standard open operation if difficulty is encountered during this procedure. This could result in a larger standard open incision and possibly a longer recuperation period.
- Failure to Remove the Stone: There is a possibility that the stone(s) may not be able to be removed completely, usually either due to the size or location of the stone(s). Additional treatment may be required.
Can kidney stones be prevented?
Prevention of kidney stones may include a combination of lifestyle changes and medications.
Lifestyle changes
You may reduce your risk of kidney stones if you:
- Drink water throughout the day.For people with a history of kidney stones, doctors usually recommend passing about 2.5 liters of urine a day. Your doctor may ask that you measure your urine output to make sure that you’re drinking enough water.
If you live in a hot, dry climate or you exercise frequently, you may need to drink even more water to produce enough urine. If your urine is light and clear, you’re likely drinking enough water.
- Eat fewer oxalate-rich foods.If you tend to form calcium oxalate stones, your doctor may recommend restricting foods rich in oxalates. These include rhubarb, beets, okra, spinach, Swiss chard, sweet potatoes, nuts, tea, chocolate and soy products.
- Choose a diet low in salt and animal protein.Reduce the amount of salt you eat and choose nonanimal protein sources, such as legumes. Consider using a salt substitute, such as Mrs. Dash.
Continue eating calcium-rich foods, but use caution with calcium supplements. Calcium in food doesn’t have an effect on your risk of kidney stones. Continue eating calcium-rich foods unless your doctor advises otherwise.Ask your doctor before taking calcium supplements, as these have been linked to increased risk of kidney stones. You may reduce the risk by taking supplements with meals. Diets low in calcium can increase kidney stone formation in some people.
Restrict the intake of red meat, organ meats and shellfish.To prevent uric acid stones, cut down on high-purine foods such as red meat, organ meats, and shellfish, and follow a healthy diet that contains mostly vegetables and fruits, whole grains, and low fat dairy products.


