Peritoneal dialysis is a way to remove waste products from your blood when your kidneys can no longer do the job adequately.In peritoneal dialysis, the lining of your abdomen or belly(peritoneum) is used, to filter your blood inside your body.
When is peritoneal dialysis required?
Dialysis is required if your kidneys don’t function adequately on their own. Kidney damage generally progresses over a number of years as a result of long-term conditions, such as:
- Diabetes
- High blood pressure (hypertension)
- Kidney inflammation (glomerulonephritis)
- Multiple cysts in the kidneys (polycystic kidney disease)
Peritoneal dialysis differs from hemodialysis, a more commonly used blood-filtering procedure. With peritoneal dialysis, you can give yourself treatments at home, at work or while traveling.
Peritoneal dialysis isn’t an option for everyone with kidney failure. You need manual dexterity and the ability to care for yourself at home, or a reliable caregiver.
Which type of dialysis is the most suitable for me?
Your doctor will discuss with you the type of dialysis that’s best for you. Factors to consider include:
- Your kidney function, as measured by blood and urine tests
- Your overall health
- Your personal preferences
- Your home situation
Peritoneal dialysis may be the better option if you:
- Can’t tolerate the rapid changes of fluid balance associated with hemodialysis
- Want to minimize the disruption of your daily activities, and work or travel more easily
- Have some residual kidney function
Peritoneal dialysis might not work if you have:
- Extensive surgical scars in your abdomen
- A large area of weakened abdominal muscle (hernia)
- Limited ability to care for yourself, or a lack of caregiving support
- Inflammatory bowel disease or frequent bouts of diverticulitis
- Protein malnutrition
- Critical illness
Most people who start dialysis with peritoneal dialysis will eventually experience a decline in kidney function and will need hemodialysis or kidney transplant.
What happens during peritoneal dialysis?
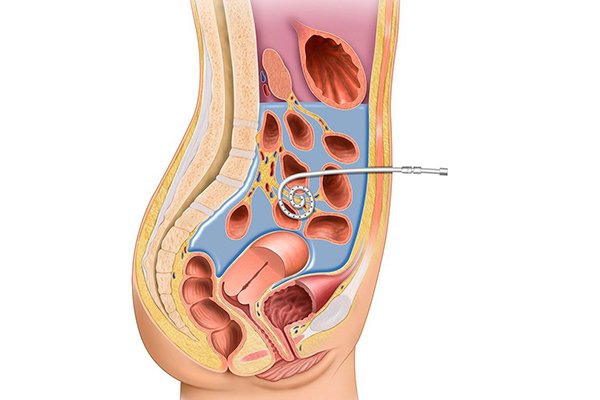
A cleansing fluid flows through a tube (catheter) into part of your abdomen and filters waste products from your blood. After a prescribed period of time, the fluid with filtered waste products flows out of your abdomen and is discarded.
The benefits of peritoneal dialysis compared with hemodialysis can include:
- Greater lifestyle flexibility and independence.These can be especially important if you work, travel or live far from a hemodialysis center.
- More flexible dietary guidelines.Peritoneal dialysis is done more continuously than hemodialysis, resulting in less accumulation of potassium, sodium and fluid.
- More stable blood chemistry and body hydration.Peritoneal dialysis doesn’t require intravenous (IV) access, which can disrupt your circulation and fluid levels.
- Longer lasting residual kidney function.People who use peritoneal dialysis might retain kidney function slightly longer than people who use hemodialysis.
How do I prepare for peritoneal dialysis?
- Surgery to put in your catheter
- Before your first treatment, you will have surgery to place a catheter into your belly. Planning your catheter placement at least 3 weeks before your first exchange can improve treatment success.
- Although you can use the catheter for dialysis as soon as it’s in place, the catheter tends to work better when you have 10 to 20 days to heal before starting a full schedule of exchanges.
- Your surgeon will make a small cut, often below and a little to the side of your belly button, and then guide the catheter through the slit into your peritoneal cavity. You’ll receive general or local anesthesia, and you may need to stay overnight in the hospital. However, most people can go home after the procedure.
- During peritoneal dialysis
- The dialysate flows into your abdomen and stays there for a prescribed period of time (dwell time) — usually four to six hours
- Dextrose in the dialysate helps filter waste, chemicals and extra fluid in your blood from tiny blood vessels (capillaries) in the lining of your abdominal cavity (peritoneum)
- When the dwell time is over, the solution — along with waste products drawn from your blood — drains into a sterile collection bag
The process of filling and then draining your abdomen is called an exchange. Different methods of peritoneal dialysis have different schedules of exchange. The two main schedules are:
- Continuous ambulatory peritoneal dialysis (CAPD)
- Continuous cycling peritoneal dialysis (CCPD)
The main differences between the two types of peritoneal dialysis are
- the schedule of exchanges
- one uses a machine and the other is done by hand
If one type of peritoneal dialysis doesn’t suit you, talk with your doctor about trying the other type.
Continuous ambulatory peritoneal dialysis (CAPD)
You fill your abdomen with dialysate, let it remain there for a prescribed dwell time, then drain the fluid. Gravity moves the fluid through the catheter and into and out of your abdomen.
With CAPD:
- You may need three to five exchanges during the day and one with a longer dwell time while you sleep
- You can do the exchanges at home, work or any clean place
- You’re free to go about your normal activities while the dialysate dwells in your abdomen
Continuous cycling peritoneal dialysis (CCPD)
Also known as automated peritoneal dialysis (APD), this method uses a machine (automated cycler) that performs multiple exchanges at night while you sleep. The cycler automatically fills your abdomen with dialysate, allows it to dwell there and then drains it to a sterile bag that you empty in the morning.
With CCPD:
- You must remain attached to the machine for 10 to 12 hours at night.
- You aren’t connected to the machine during the day. But in the morning you begin one exchange with a dwell time that lasts the entire day.
- You might have a lower risk of peritonitis because you connect and disconnect to the dialysis equipment less frequently than you do with CAPD.
- To determine the method of exchange that’s best for you, your doctor will consider your medical condition, lifestyle and personal preferences. Your doctor might suggest certain modifications to individualize your program.
What are the factors that determine the success of peritoneal dialysis?
Many factors affect how well peritoneal dialysis works in removing wastes and extra fluid from your blood. These factors include:
- Your size
- How quickly your peritoneum filters waste
- How much dialysis solution you use
- The number of daily exchanges
- Length of dwell times
- The concentration of sugar in the dialysis solution
To check if your dialysis is removing enough waste products, your doctor is likely to recommend:
- Peritoneal equilibration test (PET).This test compares samples of your blood and your dialysis solution during an exchange. The results indicate whether waste toxins pass quickly or slowly from your blood into the dialysate. That information helps determine whether your dialysis would be improved if the solution stayed in your abdomen for a shorter or longer time.
- Clearance test.A blood sample and a sample of used dialysis solution are analyzed to determine how much of a certain waste product (urea) is being removed from your blood during dialysis. If you still produce urine, your doctor may also take a urine sample to measure its urea concentration.
If the test results show that your dialysis schedule is not removing enough wastes, your doctor might change your dialysis routine to:
- Increase the number of exchanges
- Increase the amount of dialysate you use for each exchange
- Use a dialysate with a higher concentration of dextrose
What are the possible problems from peritoneal dialysis?
Possible problems from peritoneal dialysis include infection, hernia, and weight gain
Infections. One of the most serious problems related to peritoneal dialysis is infection. You can get an infection of the skin around your catheter exit site or you can develop peritonitis, an infection in the fluid in your belly. Bacteria can enter your body through your catheter as you connect or disconnect it from the bags.Seek immediate care if you have signs of infection
Signs of an exit site infection include redness, pus, swelling or bulging, and tenderness or pain at the exit site. Health care professionals treat infections at the exit site with antibiotics.
Peritonitis may cause
- pain in the abdomen
- fever
- nauseaor vomiting
- redness or pain around your catheter
- unusual color or cloudiness in used dialysis solution
- the catheter cuff to push out from your body—the cuff is the part of the catheter that holds it in place
Health care professionals treat peritonitis with antibiotics. Antibiotics are added to the dialysis solution that you can usually take at home. Quick treatment may prevent additional problems.
Weight gain. The dialysate contains sugar (dextrose). Absorbing some of the dialysate might cause you to take in several hundred extra calories a day, leading to weight gain. The extra calories can also cause high blood sugar, especially if you have diabetes.Your dietitian can provide helpful guidance to reduce weight gain.
Hernia. A hernia is an area of weakness in your abdominal muscle.Peritoneal dialysis increases your risk for a hernia for a couple of reasons. First, you have an opening in your muscle for your catheter. Second, the weight of the dialysis solution within your belly puts pressure on your muscle. Hernias can occur near your belly button, near the exit site, or in your groin. If you have a swelling or new lump in your groin or belly, talk with your health care professional.
Inadequate dialysis. Peritoneal dialysis can become ineffective after several years. You might need to switch to hemodialysis.
What care do I need to take while I am on peritoneal dialysis?
If you’re on peritoneal dialysis, you may need to limit
- sodium
- phosphorus
- caloriesin your eating plan
You may also need to
- watch how much liquid you drink and eat. Your dietitianwill help you determine how much liquid you need to consume each day.
- add proteinto your diet because peritoneal dialysis removes protein.
- choose foods with the right amount of potassium.
- take supplements made for people with kidney failure.
Eating the right foods can help you feel better while you’re on peritoneal dialysis. Talk with your dialysis center’s dietitian to find a meal plan that works for you.
If you have peritoneal dialysis, you’ll need to avoid:
- Certain prescription and over-the-counter medications that can damage your kidneys, including nonsteroidal anti-inflammatory drugs.
- Soaking in a bath or hot tub, or swimming in a lake, pond, river or nonchlorinated pool — which increases the risk of infection. Showers and swimming in a chlorinated pool are generally acceptable.