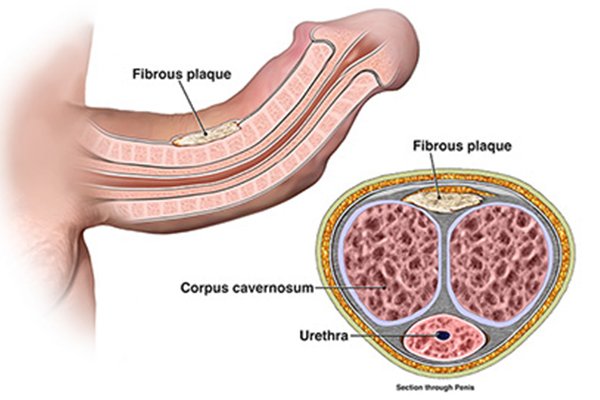
Peyronie’s disease is a disorder in which scar tissue, called a plaque, forms in the penis—the male organ used for urination and sex. The plaque builds up inside the tissues of a thick, elastic membrane called the tunica albuginea. The most common area for the plaque is on the top or bottom of the penis. As the plaque builds up, the penis will curve or bend, which can prevent a man from having sexor might make it difficult to get or maintain an erection (erectile dysfunction) or cause painful erections. Peyronie’s disease begins with inflammation, or swelling, which can become a hard scar.Peyronie’s disease is not contagious or caused by any known transmittable disease.
Causes
Medical experts do not know the exact cause of Peyronie’s disease. Many believe that Peyronie’s disease may be the result of
- acute injury to the penis
- chronic, or repeated, injury to the penis
- autoimmune disease—a disorder in which the body’s immune system attacks the body’s own cells and organs
1. Injury to the Penis
Medical experts believe that hitting or bending the penis may injure the tissues inside. A man may injure the penis during sex, athletic activity, or an accident. Injury ruptures blood vessels, which leads to bleeding and swelling inside the layers of the tunica albuginea. Swelling inside the penis will block blood flow through the layers of tissue inside the penis. When the blood cannot flow normally, clots can form and trap immune system cells. As the injury heals, the immune system cells may release substances that lead to the formation of too much scar tissue. The scar tissue builds up and forms a plaque inside the penis. The plaque reduces the elasticity of tissues and flexibility of the penis during erection, leading to curvature. The plaque may further harden because of calcification––the process in which calcium builds up in body tissue.
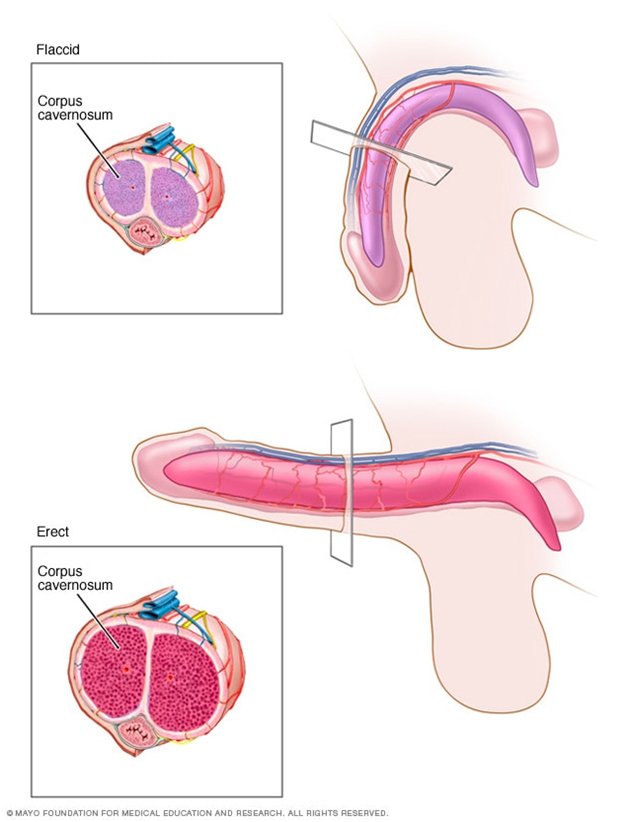
Each side of the penis contains a sponge-like tube (corpus cavernosum) that contains many tiny blood vessels. Each of the corpora cavernosa is encased in a sheath of elastic tissue called the tunica albuginea which stretches during an erection.When a man becomes sexually aroused, blood flow to these chambers increases. As the chambers fill with blood, the penis expands, straightens and stiffens into an erection.In Peyronie’s disease, when the penis becomes erect, the region with the scar tissue doesn’t stretch, and the penis bends or becomes disfigured and possibly painful.
In some men, Peyronie’s disease comes on gradually and doesn’t seem to be related to an injury. Researchers are investigating whether Peyronie’s disease might be linked to an inherited trait or certain health conditions.
1. Autoimmune Disease
Some medical experts believe that Peyronie’s disease may be part of an autoimmune disease. Normally, the immune system is the body’s way of protecting itself from infection by identifying and destroying bacteria, viruses, and other potentially harmful foreign substances. Men who have autoimmune diseases may develop Peyronie’s disease when the immune system attacks cells in the penis. This can lead to inflammation in the penis and can cause scarring. Medical experts do not know what causes autoimmune diseases. Some of the autoimmune diseases associated with Peyronie’s disease affect connective tissues. Connective tissue is specialized tissue that supports, joins, or separates different types of tissues and organs of the body.
Risk factors
The following factors may increase a man’s chance of developing Peyronie’s disease:
- vigorous sexual or nonsexual activities that cause microscopic injury to the penis
- certain connective tissue and autoimmune disorders
- a family history of Peyronie’s disease
- aging
i. Vigorous Sexual and Nonsexual Activities
Men whose sexual or nonsexual activities cause microscopic injury to the penis are more likely to develop Peyronie’s disease.
ii. Connective Tissue and Autoimmune Disorders
Men who have certain connective tissue and autoimmune disorders may have a higher chance of developing Peyronie’s disease. A common example is a condition known as Dupuytren’s disease, an abnormal cordlike thickening across the palm of the hand. Dupuytren’s disease is also known as Dupuytren’s contracture. Although Dupuytren’s disease is fairly common in older men, only about 15 percent of men with Peyronie’s disease will also have Dupuytren’s disease.Other connective tissue disorders associated with Peyronie’s disease include
- plantar fasciitis––inflammation of the plantar fascia, thick tissue on the bottom of the foot that connects the heel bone to the toes and creates the arch of the foot
- scleroderma––abnormal growth of connective tissue, causing it to get thick and hard; scleroderma can cause swelling or pain in muscles and joints
Autoimmune disorders associated with Peyronie’s disease include
- systemic lupus erythematosus––inflammation and damage to various body tissues, including the joints, skin, kidneys, heart, lungs, blood vessels, and brain
- Sjögren’s syndrome––inflammation and damage to the glands that make tears and saliva
- Behcet’s syndrome––inflammation of the blood vessels
iii. Family History of Peyronie’s Disease
Medical experts believe that Peyronie’s disease may run in some families. For example, a man whose father or brother has Peyronie’s disease may have an increased chance of getting the disease.
iv. Aging
The chance of getting Peyronie’s disease increases with age. Age-related changes in the elasticity of tissues in the penis may cause it to be more easily injured and less likely to heal well.
Signs and symptoms
Peyronie’s disease signs and symptoms might appear suddenly or develop gradually. Symptoms of Peyronie’s disease range from mild to severe. The most common signs and symptoms include:
- Scar tissue. The scar tissue (plaques) associated with Peyronie’s disease can be felt under the skin of the penis as flat lumps or a band of hard tissue.
- A significant bend to the penis.The penis might be curved upward, downward or bent to one side. In some cases, the erect penis might have narrowing, indentations or an hourglass appearance, with a tight, narrow band around the shaft.
- Erection problems.Peyronie’s disease might cause problems getting or maintaining an erection (erectile dysfunction).
- Shortening of the penis.The penis might become shorter as a result of Peyronie’s disease.
- Pain.A man with Peyronie’s disease might have penile pain, with or without an erection.In many cases, the pain decreases over time, although the curve in the penis may remain.
Complications
Complications of Peyronie’s disease may include:
- the inability to have sexual intercourse
- erectile dysfunction (difficulty achieving or maintaining an erection)
- anxiety, or stress, about sexual abilities or the appearance of the penis
- stress on a relationship with a sexual partner
- problems fathering a child because intercourse is difficult or impossible
Diagnosis
A urologist diagnoses Peyronie’s disease based on the following:
- a medical and family history
- a physical exam
- imaging tests
1. Medical and Family History
Taking a medical and family history is one of the first things a urologist may do to help diagnose Peyronie’s disease. He or she will ask the man to provide a medical and family history, which may include the following questions:
- What is the man’s ability to have an erection?
- What are the problems with sexual intercourse?
- When did the symptoms begin?
- What is the family medical history?
- What medications is the man taking?
- What other symptoms is the man experiencing?
- What other medical conditions does the man have?
2. Physical Exam
A physical exam may help diagnose Peyronie’s disease. During a physical exam, a urologist usually examines the man’s body, including the penis.
A urologist can usually feel the plaque in the penis with or without an erection. Sometimes the urologist will need to examine the penis during an erection. The urologist will give the man an injectable medication to cause an erection.
3. Imaging Tests
To help pinpoint the location of the plaque buildup inside the penis, a urologist may perform
- ultrasound of the penis
- an x-ray of the penis
For both tests, a specially trained technician performs the procedure in a health care provider’s office, an outpatient center, or a hospital, and a radiologist—a doctor who specializes in medical imaging—interprets the images. The patient does not need anesthesia.
Ultrasound. Ultrasound uses a device, called a transducer, that bounces safe, painless sound waves off organs to create an image of their structure.
X-ray. An x-ray is a picture created by using radiation and recorded on film or on a computer. The amount of radiation used is small. The man will lie on a table or stand during the x-ray, and the technician may ask the man to change positions for additional pictures.
Treatment
The goal of treatment is to reduce pain and restore and maintain the ability to have intercourse. Men with small plaques, minimal penile curvature, no pain, and satisfactory sexual function may not need treatment until symptoms get worse. Peyronie’s disease often resolves on its own without treatment.
Your doctor might recommend a wait-and-see (watchful waiting) approach if:
- The curvature of your penis is not severe and is no longer worsening
- You can still have erections and sex with no or mild pain
- You have good erectile function
If your symptoms are severe or are worsening over time, your doctor might recommend medication or surgery.
1. Lifestyle Changes
A man can make healthy lifestyle changes to reduce the chance of erectile dysfunction associated with Peyronie’s disease by
- quitting smoking
- reducing alcohol consumption
- exercising regularly
- avoiding illegal drugs
2. Medications
A number of oral medications have been tried to treat Peyronie’s disease, but they have not been shown to be effective consistently and are not as effective as surgery.
In some cases, drugs injected directly into the penis might reduce curvature and pain associated with Peyronie’s disease. Depending on the therapy, you might be given a local anesthetic to prevent pain during the injections.
3. Medical therapies
A urologist may use medical therapies to break up scar tissue and decrease plaque size and curvature. Therapies to break up scar tissue may include
- high-intensity, focused ultrasound directed at the plaque
- radiation therapy––high-energy rays, such as x-rays, aimed at the plaque
- shockwave therapy––focused, low-intensity electroshock waves directed at the plaque
- iontophoresis––painless, low-level electric current that delivers medications through the skin over the plaque––to decrease plaque size and curvature
- mechanical traction and vacuum devices aimed at stretching or bending the penis to reduce curvature.
4. Surgery
A urologist may recommend surgery to remove plaque or help straighten the penis during an erection. Medical experts recommend surgery for long-term cases when
- symptoms have not improved
- erections, intercourse, or both are painful
- the curve or bend in the penis does not allow the man to have sexual intercourse
Some men may develop complications after surgery, and sometimes surgery does not correct the effects of Peyronie’s disease––such as shortening of the penis. Some surgical methods can cause shortening of the penis. Medical experts suggest waiting 1 year or more from the onset of symptoms before having surgery because the course of Peyronie’s disease is different in each man.
A urologist may recommend the following surgeries:
- penile implants.A urologist implants a device into the penis that can cause an erection and help straighten it during an erection. Penile implants may be considered if a man has both Peyronie’s disease and erectile dysfunction. In some cases, an implant alone will straighten the penis adequately. If the implant alone does not straighten the penis, a urologist may combine implantation with one of the other two surgeries. Once a man has an implant, he must use the device to have an erection.
- plication.A urologist will remove or pinch a piece of the tunica albuginea from the side of the penis opposite the plaque, which helps to straighten the penis. This procedure is less likely to cause numbness or erectile dysfunction. Plication cannot restore length or girth of the penis and may cause shortening of the penis.
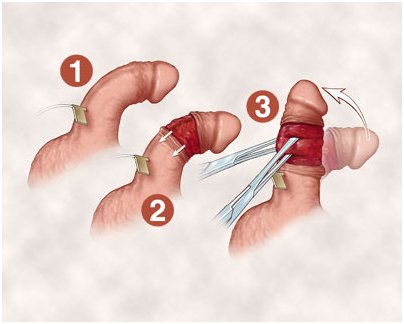
Nesbit plication
- Incision or excision and grafting.A urologist will cut or remove the plaque and attach a patch of skin, a vein, or material made from animal organs in its place. This procedure may straighten the penis and restore some lost length from Peyronie’s disease. However, some men may experience numbness of the penis and erectile dysfunction after the procedure.This procedure is generally used in cases of more-severe curvature or deformity, such as indentations. This procedure is associated with greater risks of worsening erectile function when compared to the plication procedures.
Depending on the type of surgery you have, you might be able to go home from the hospital the same day or you might need to stay overnight. Your surgeon will advise you on how long you should wait before going back to work — in most cases, a few days. After surgery for Peyronie’s disease, you’ll need to wait four to eight weeks before sexual activity.